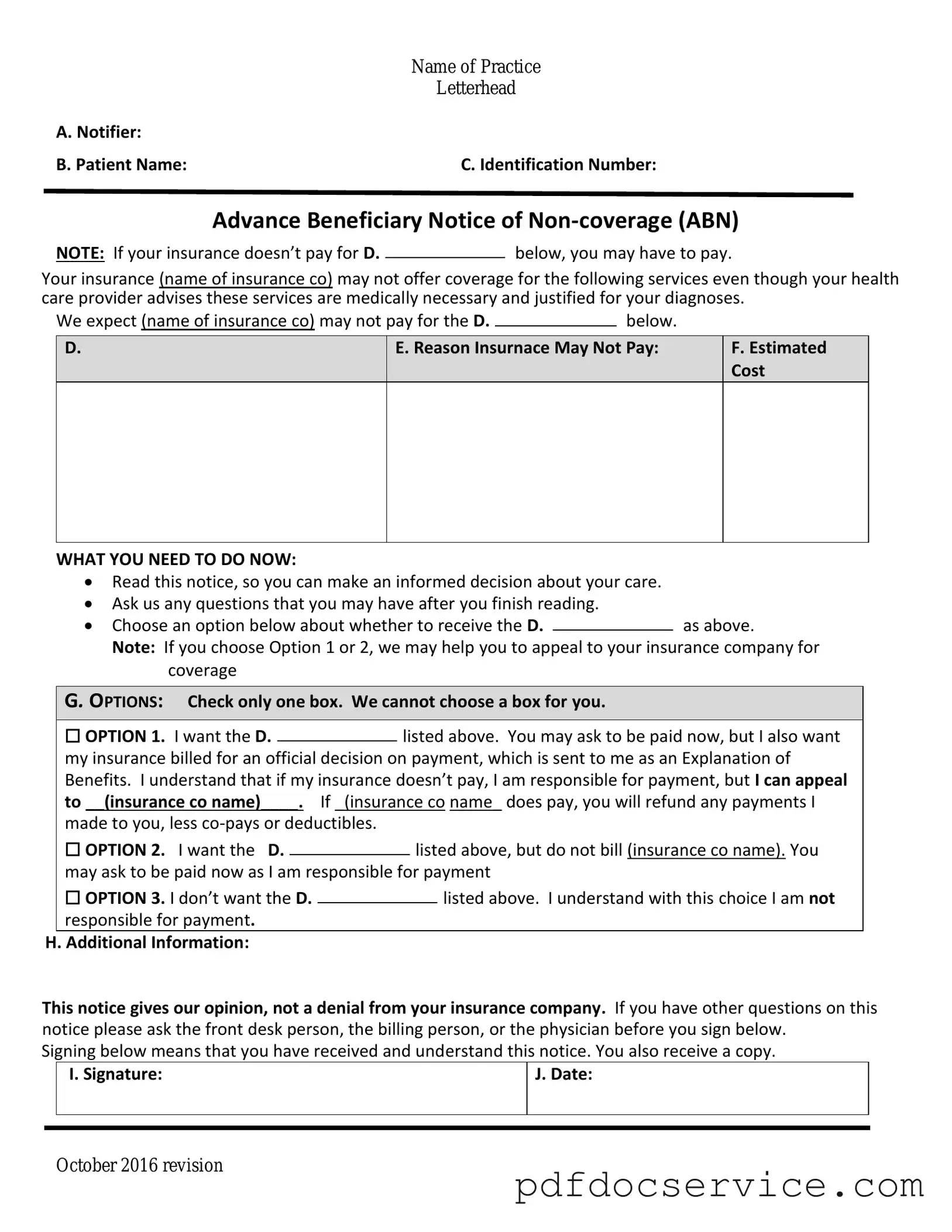
Fill Your Advance Beneficiary Notice of Non-coverage Form
The Advance Beneficiary Notice of Non-coverage (ABN) is a crucial document that informs Medicare beneficiaries when a service or item may not be covered by Medicare. By providing this notice, healthcare providers help patients understand their potential financial responsibility before receiving care. This proactive communication ensures that individuals can make informed decisions about their healthcare options.
Open Advance Beneficiary Notice of Non-coverage Editor
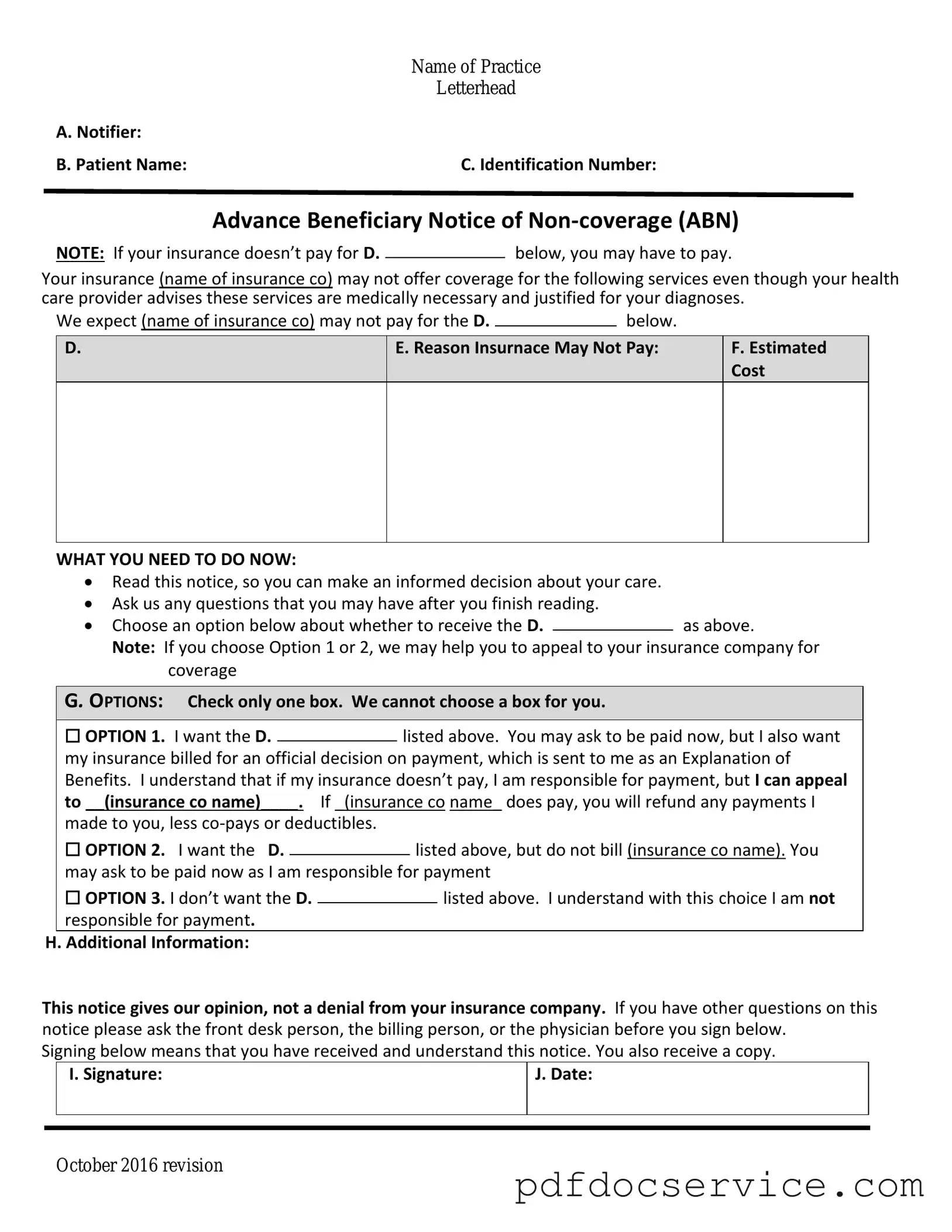
Fill Your Advance Beneficiary Notice of Non-coverage Form
Open Advance Beneficiary Notice of Non-coverage Editor
Open Advance Beneficiary Notice of Non-coverage Editor
or
Get Advance Beneficiary Notice of Non-coverage PDF
Finish the form now and be done
Finish Advance Beneficiary Notice of Non-coverage online using simple edit, save, and download steps.