Fill Your Annual Physical Examination Form
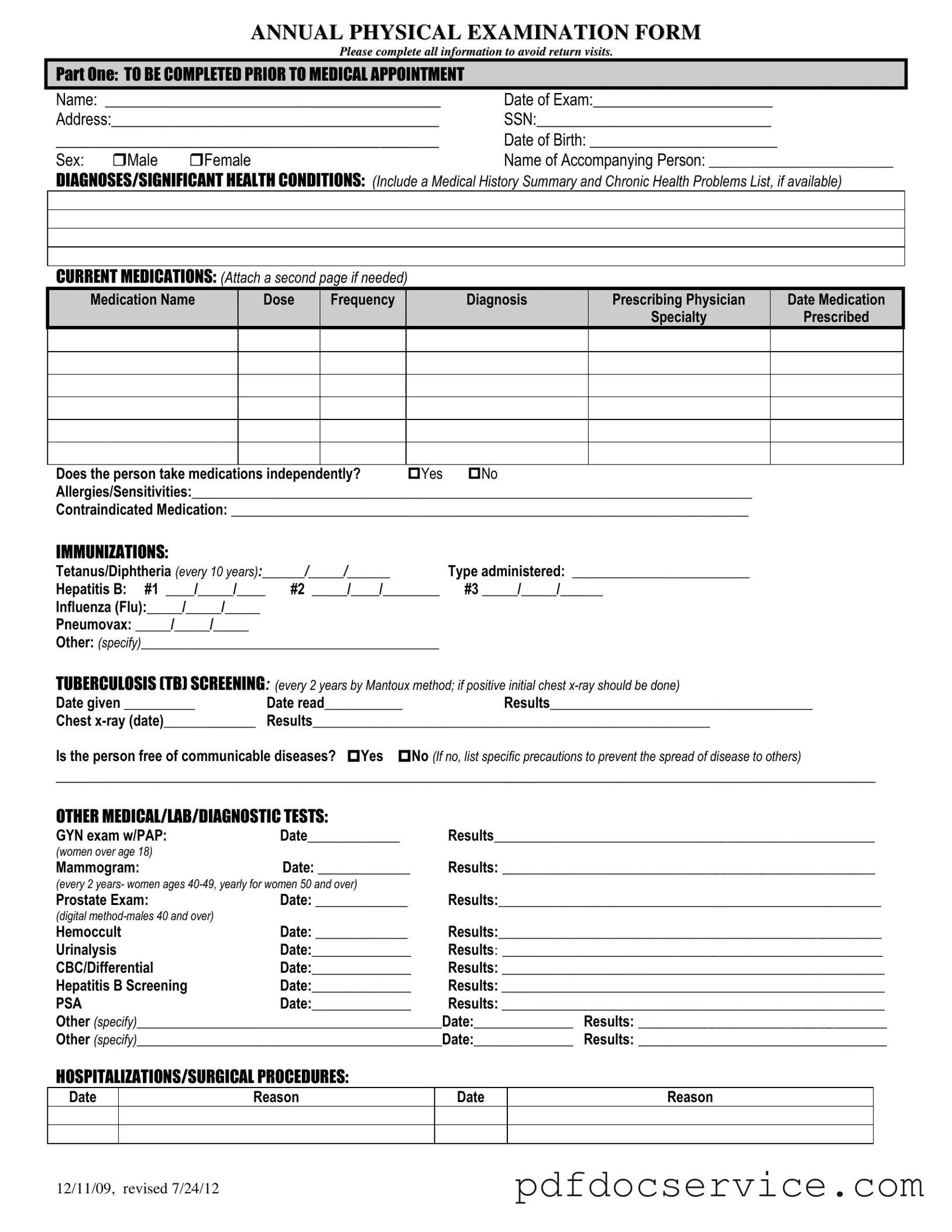
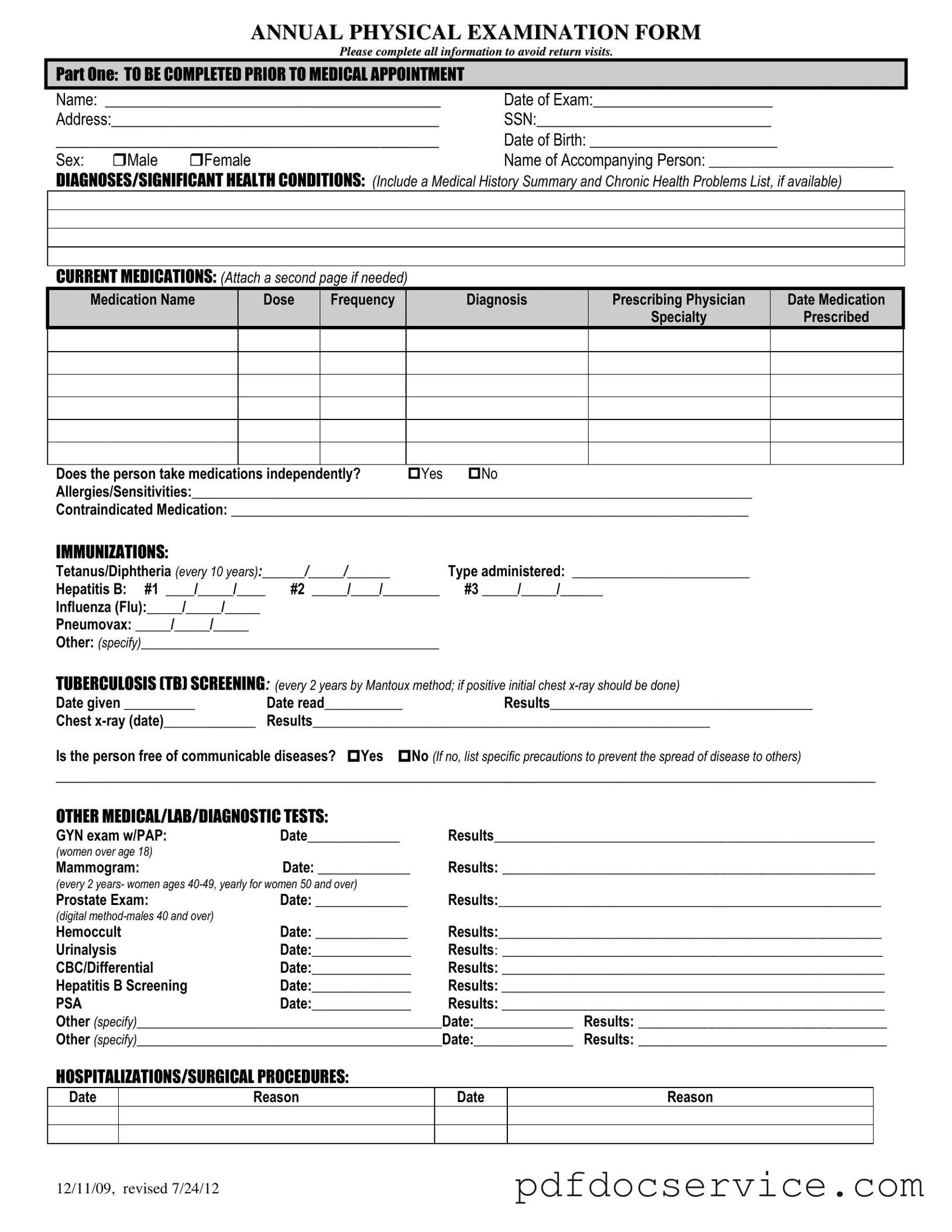
The Annual Physical Examination form is a crucial document designed to collect comprehensive health information prior to a medical appointment. This form ensures that healthcare providers have all necessary details to deliver effective care and address any significant health concerns. Completing this form accurately helps to streamline the examination process and fosters better communication between patients and their healthcare teams.
Open Annual Physical Examination Editor
Fill Your Annual Physical Examination Form
Open Annual Physical Examination Editor
Open Annual Physical Examination Editor
or
Get Annual Physical Examination PDF
Finish the form now and be done
Finish Annual Physical Examination online using simple edit, save, and download steps.