What is a Do Not Resuscitate (DNR) Order?
A Do Not Resuscitate Order is a legal document that allows individuals to refuse certain medical interventions, specifically cardiopulmonary resuscitation (CPR), in the event of a cardiac arrest or respiratory failure. This order is typically used by patients who have a terminal illness or a condition that significantly impacts their quality of life.
Who can request a DNR Order?
Generally, any competent adult can request a DNR Order. This includes patients who understand the implications of the order and wish to make their preferences known. Additionally, a legal guardian or healthcare proxy may request a DNR on behalf of an incapacitated individual.
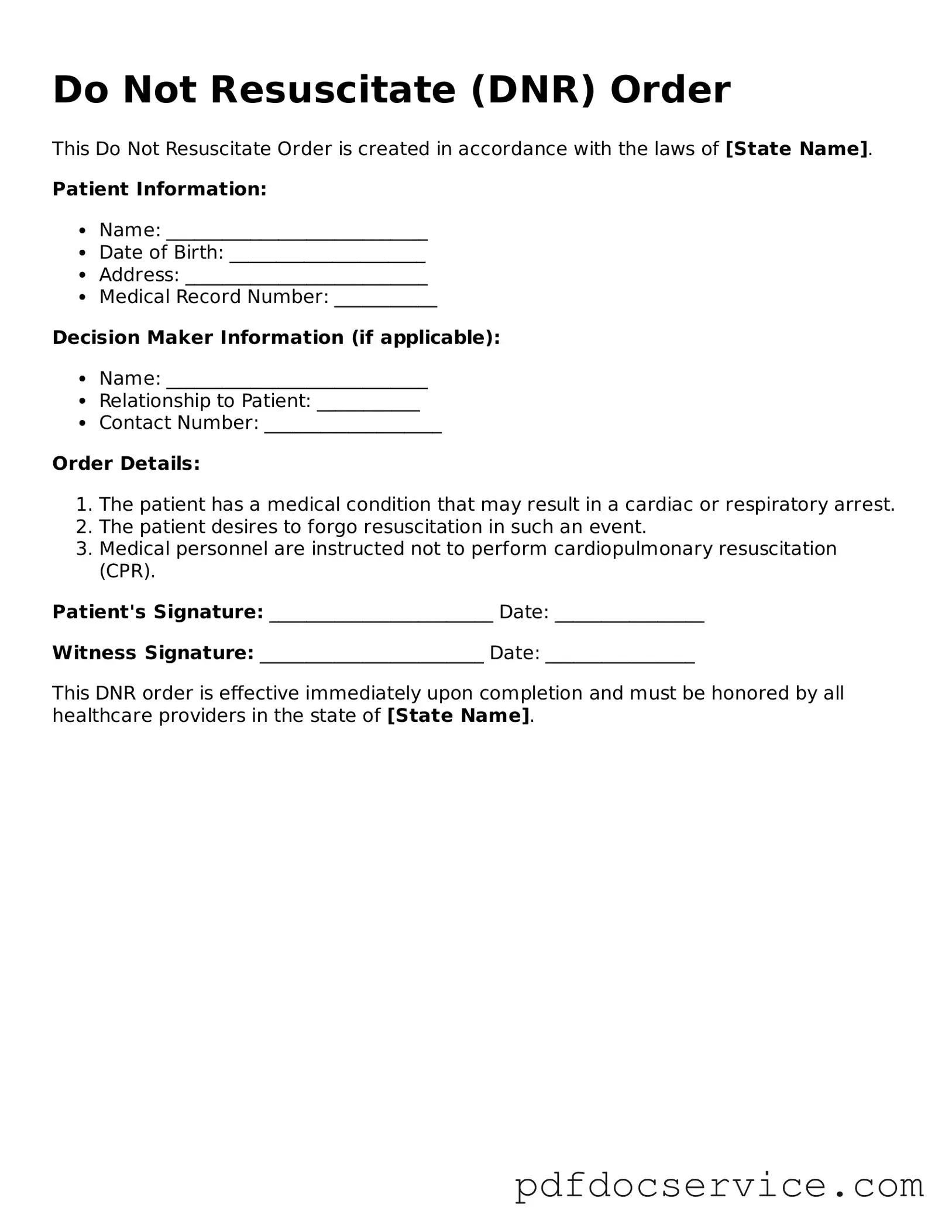
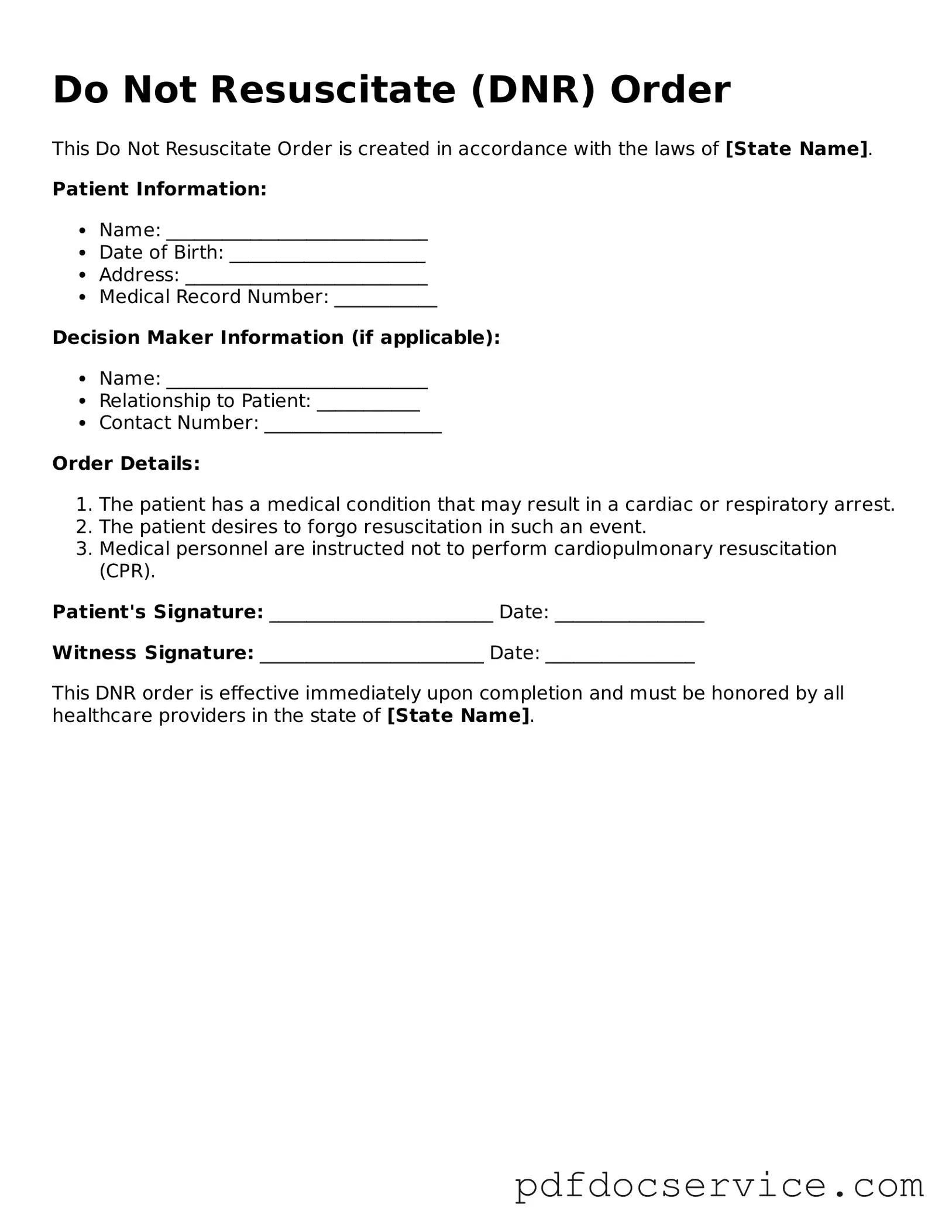
How is a DNR Order created?
To create a DNR Order, a patient must typically fill out a specific form provided by their state or healthcare provider. This form often requires the signature of the patient, their physician, and sometimes a witness. It's important to consult with a healthcare professional to ensure that the order complies with state laws.
Where should I keep my DNR Order?
It is crucial to keep your DNR Order in a place that is easily accessible to both you and your healthcare providers. Common recommendations include:
-
Carrying a copy in your wallet or purse.
-
Keeping a copy in your medical records.
-
Displaying a copy prominently in your home, such as on the refrigerator.
Can a DNR Order be revoked?
Yes, a DNR Order can be revoked at any time by the patient or their legal representative. This can be done verbally or in writing. It is advisable to inform your healthcare providers and family members of any changes to ensure that your current wishes are known.
What happens if a DNR Order is not honored?
If a DNR Order is not honored, it can lead to unwanted medical interventions, which may go against the patient’s wishes. In such cases, family members or representatives may need to advocate for the patient’s preferences. Legal recourse is available, but it can be a complex and emotional process.
Are there different types of DNR Orders?
Yes, there are different types of DNR Orders, which may vary by state. Some states have specific forms for hospital settings, while others may have out-of-hospital DNR Orders. It is essential to understand the distinctions and ensure that the correct form is used based on the patient’s circumstances.
How does a DNR Order affect other medical treatments?
A DNR Order specifically addresses resuscitation efforts during a medical emergency. It does not affect other treatments, such as pain management, comfort care, or life-sustaining measures that do not involve resuscitation. Patients should discuss their overall healthcare preferences with their medical team.
Can family members override a DNR Order?
Generally, family members cannot override a DNR Order if the patient is competent and has made their wishes clear. However, if the patient is incapacitated, family members may have the authority to make decisions based on what they believe the patient would want. It is crucial to have open discussions about these wishes to avoid confusion during critical moments.