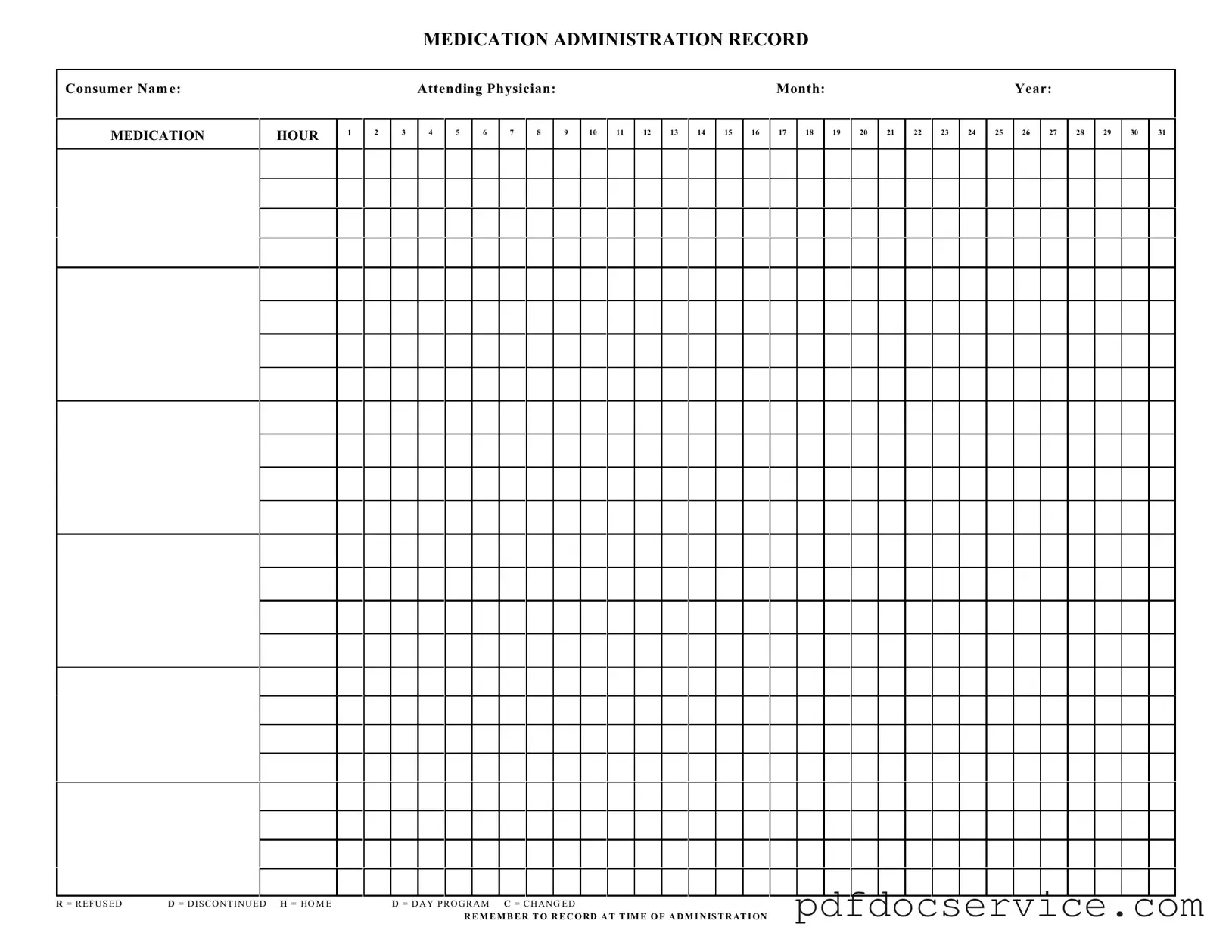
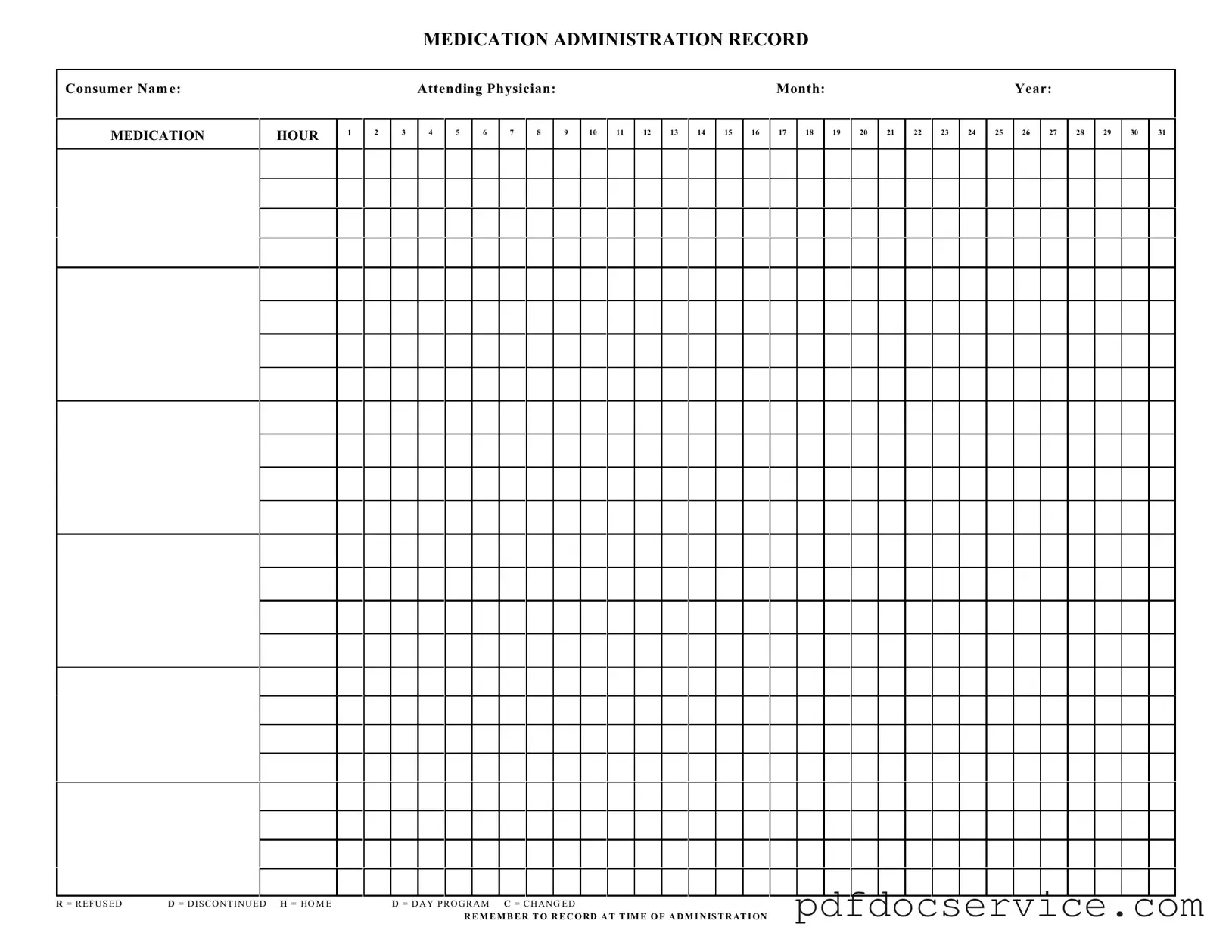
What is a Medication Administration Record Sheet?
The Medication Administration Record Sheet is a crucial document used in healthcare settings to track the administration of medications to patients. It provides a detailed log of when and how medications are given, ensuring that patients receive their prescribed treatments accurately and on time.
Who should use the Medication Administration Record Sheet?
This form should be utilized by healthcare professionals involved in administering medications, including nurses, caregivers, and pharmacists. It is essential for anyone responsible for ensuring that patients adhere to their medication schedules and for maintaining accurate medical records.
The Medication Administration Record Sheet requires several key pieces of information:
-
Consumer's name
-
Attending physician's name
-
Month and year of medication administration
-
Hours of medication administration
-
Specific medications given, along with any notations such as refused or discontinued medications
How should medications be recorded on the sheet?
Medications should be recorded at the time of administration. Each hour should be marked clearly with the appropriate notation. For instance, if a medication is refused, the letter "R" should be noted. If a medication is discontinued, use "D." It is vital to maintain accuracy in these records for patient safety and compliance with healthcare regulations.
The form includes specific notations to indicate the status of medication administration:
-
R
= Refused
-
D
= Discontinued
-
H
= Home
-
D
= Day Program
-
C
= Changed
These notations help in tracking medication adherence and any changes in the patient's treatment plan.
Why is it important to record medications at the time of administration?
Recording medications at the time of administration is critical for several reasons. It ensures that there is an accurate account of what medications have been given, which helps prevent errors. Timely documentation also assists in monitoring the patient's response to medications and facilitates communication among healthcare providers.
No, the Medication Administration Record Sheet is designed for individual patient use. Each patient should have their own record to ensure that their specific medication regimen is accurately tracked and monitored. This practice promotes better patient care and safety.
What should be done if a medication is missed?
If a medication is missed, it should be documented appropriately on the Medication Administration Record Sheet. The healthcare provider should note the reason for the missed dose and take appropriate action based on the facility's policies. Communication with the attending physician may also be necessary to determine the next steps for the patient's treatment.
How can I ensure compliance with using the Medication Administration Record Sheet?
To ensure compliance, healthcare providers should receive training on the proper use of the Medication Administration Record Sheet. Regular audits and reviews of the records can help identify any discrepancies or areas for improvement. Additionally, fostering a culture of accountability and communication among staff can enhance adherence to proper medication administration practices.