Fill Your Tb Test Form
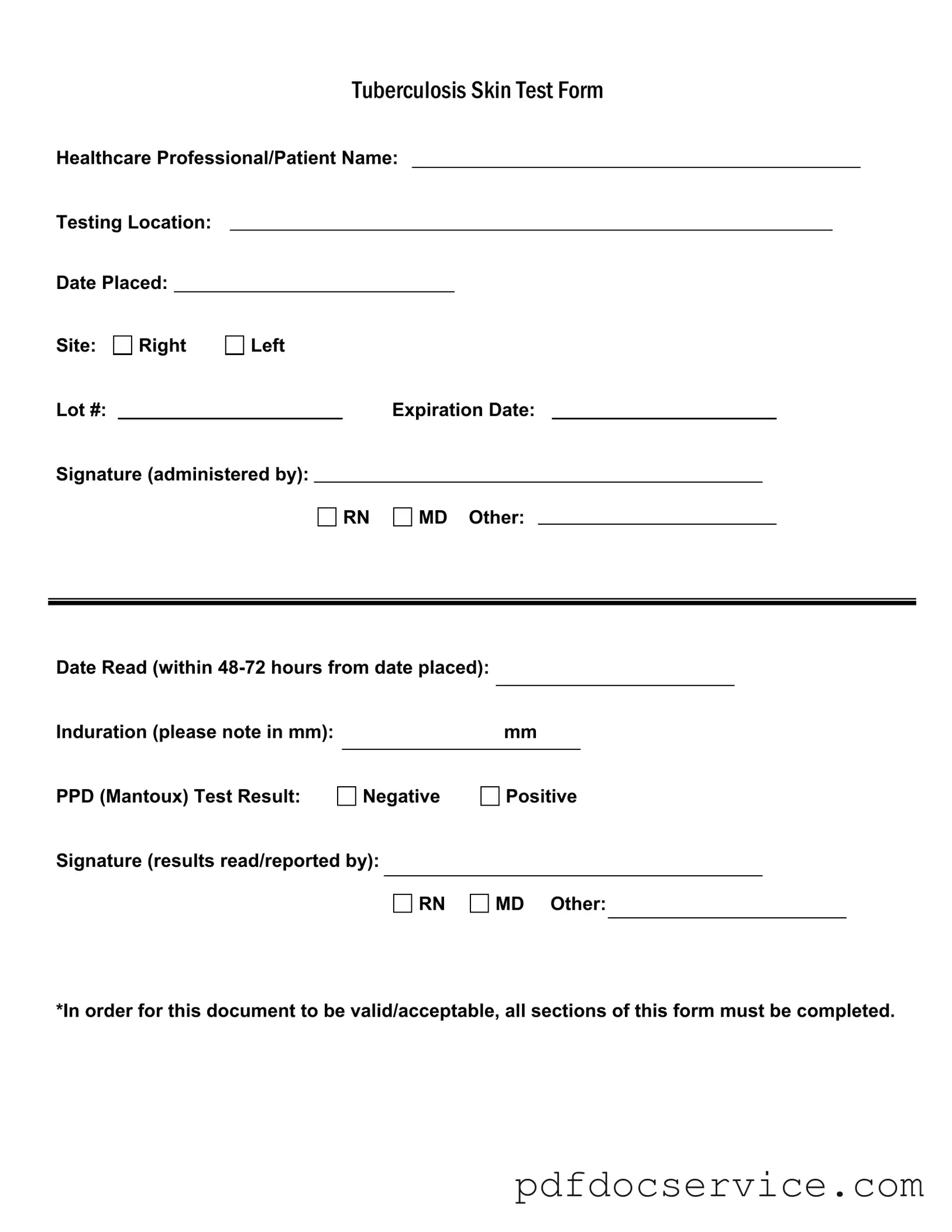
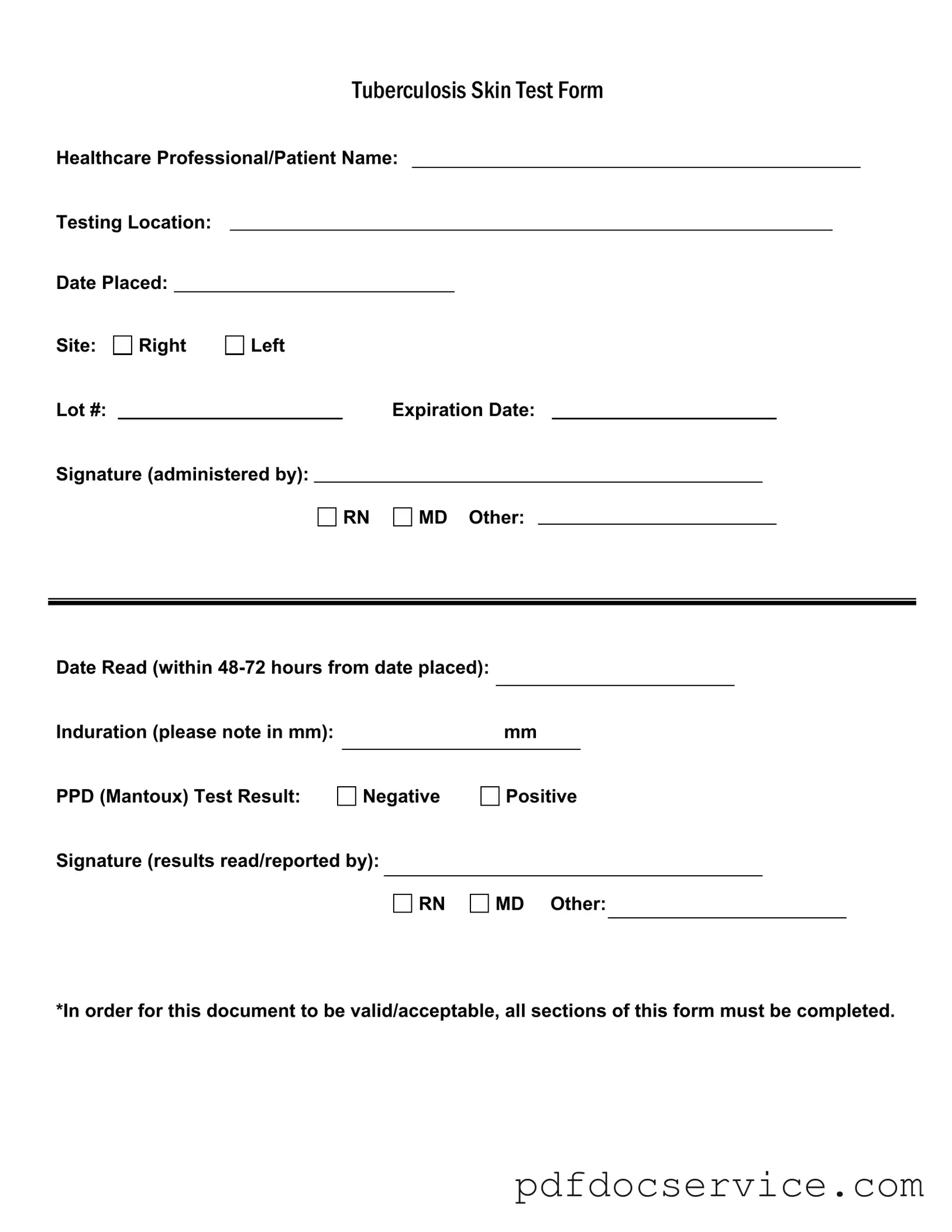
The Tuberculosis Skin Test Form is a critical document used to record the administration and results of the tuberculosis (TB) skin test, commonly known as the PPD test. This form captures essential information such as the healthcare professional's name, testing location, and the test results, ensuring that all necessary details are documented for accurate health assessments. Completing every section of the form is vital for its validity and acceptance in medical contexts.
Open Tb Test Editor
Fill Your Tb Test Form
Open Tb Test Editor
Open Tb Test Editor
or
Get Tb Test PDF
Finish the form now and be done
Finish Tb Test online using simple edit, save, and download steps.